Leprosy, an ancient disease that continues to afflict communities worldwide, often conjures images of disfiguring skin sores. However, a lesser-known form of leprosy, called pure neuritic leprosy (PNL), can inflict significant damage without any visible skin changes. This "hidden" form of leprosy, primarily affecting peripheral nerves, often goes undiagnosed, leading to delayed treatment and potential disabilities.
Now, a groundbreaking study by researchers at AIIMS Bhubaneswar has shed new light on PNL, paving the way for earlier diagnosis and targeted interventions. The study, led by Dr. Sanjeev Kumar Bhoi, Head of the Neurology Department, revealed a surprising finding: a majority of PNL cases involve subclinical involvement of the central nervous system. This means the disease can subtly affect the brain and spinal cord even without causing noticeable skin lesions.
This discovery has significant implications for leprosy diagnosis and management. Dr. Bhoi explains, "Our study shows that PNL can subtly affect the central nervous system. Such leprosy cases are often left undiagnosed due to the absence of skin-related symptoms. Testing both peripheral and central nervous involvement will definitely help detect PNL early, allowing for treatment to reduce disability risks."
The research, funded by the Odisha government, involved a comprehensive study of 76 patients suspected of having PNL. Nerve biopsies confirmed the diagnosis in 49 patients aged between 14 and 72. The study found that most patients were men, with unilateral foot drop and claw hand being the most common symptoms.
Published in the medical journal Acta Neurologica Belgica, the study recommends a new approach to PNL diagnosis:
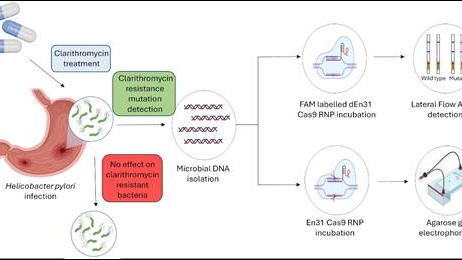
Nerve Conduction Studies: For patients with nerve-related symptoms like sensory loss or muscle weakness without skin lesions, nerve conduction studies should be conducted.
Central Nervous System Tests: Specific tests like VEP (for vision nerve pathways), SSEP (for sensory pathways), and BAEP (for auditory pathways) should be considered for a more comprehensive diagnosis.
This research challenges the conventional understanding of PNL as solely a peripheral nerve disease, highlighting the importance of assessing central nervous system involvement for early detection and treatment. Dr. Bhoi notes that many PNL patients, including those from affluent backgrounds, are often unaware they have leprosy due to the lack of visible skin symptoms.
This study marks a significant step forward in the fight against leprosy, particularly in regions like India where PNL is more prevalent. By improving diagnostic accuracy and enabling timely treatment, this research offers hope for reducing disability and improving the quality of life for those affected by this often-overlooked form of leprosy.