Thyroid problems during pregnancy can significantly impact both maternal and fetal health. Proper diagnosis and management are crucial to ensure a healthy pregnancy outcome. Here’s an overview of the risks and management strategies for thyroid issues during pregnancy.
Risks of Thyroid Problems During Pregnancy
1. Hypothyroidism:
Causes: Often due to Hashimoto's thyroiditis, an autoimmune disorder.
Maternal Risks:
Miscarriage
Preeclampsia
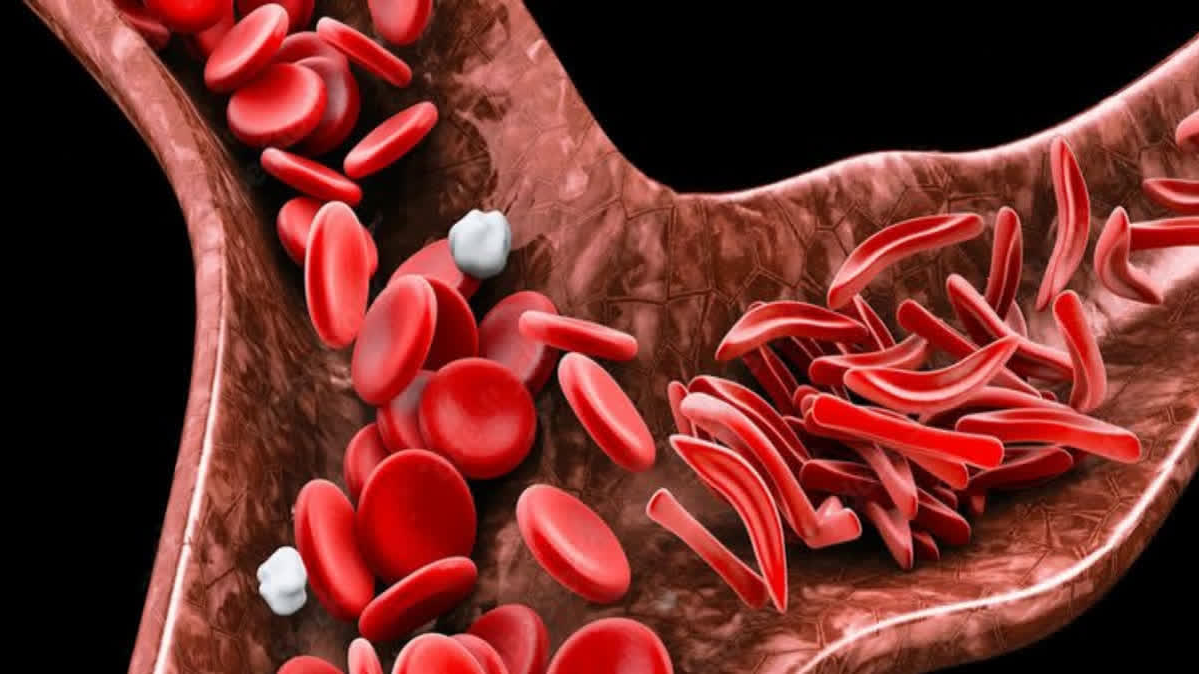
Anemia
Placental abruption
Postpartum hemorrhage
Fetal Risks:
Low birth weight
Preterm birth
Stillbirth
Neurodevelopmental delays
Congenital hypothyroidism
2. Hyperthyroidism:
Causes: Commonly due to Graves' disease, another autoimmune disorder.
Maternal Risks:
Severe nausea and vomiting (hyperemesis gravidarum)
Preeclampsia
Heart failure
Thyroid storm (a rare, life-threatening condition)
Fetal Risks:
Miscarriage
Preterm birth
Low birth weight
Fetal growth restriction
Neonatal thyrotoxicosis (excessive thyroid hormone in the newborn)
Stillbirth
Management Strategies
1. Preconception Counseling:
Women with pre-existing thyroid conditions should seek medical advice before conceiving.
Ensure thyroid function is well-controlled prior to pregnancy.
2. Screening and Diagnosis:
Initial Screening: Thyroid function tests (TSH, Free T4) early in pregnancy or preconception.
Risk Factors for Screening:
History of thyroid disease or dysfunction
Family history of thyroid disease
Presence of goiter
Symptoms of thyroid dysfunction
Type 1 diabetes or other autoimmune disorders
3. Management of Hypothyroidism:
Levothyroxine Therapy: The standard treatment, safe during pregnancy.
Dosage Adjustment: Often requires a 30-50% increase in dose due to increased thyroid hormone demand during pregnancy.
Monitoring: Regular TSH and Free T4 levels every 4-6 weeks to adjust dosage.
Nutritional Support:
Adequate iodine intake is crucial for thyroid function.
Prenatal vitamins typically contain sufficient iodine.
4. Management of Hyperthyroidism:
Antithyroid Medications: Propylthiouracil (PTU) is preferred during the first trimester, switching to methimazole in the second and third trimesters.
Monitoring: Regular thyroid function tests to adjust medication dosage.
Beta-blockers: May be used short-term to manage symptoms like palpitations and tremors.
Surgical Intervention: Rarely necessary; thyroidectomy is considered if medication is ineffective or not tolerated.
Radioactive Iodine: Contraindicated during pregnancy.
5. Monitoring and Follow-up:
Frequent thyroid function tests throughout pregnancy.
Close collaboration between obstetricians, endocrinologists, and primary care providers.
Adjustments in medication dosages based on trimester-specific reference ranges for TSH and Free T4.
6. Postpartum Care:
Hypothyroidism: Monitor thyroid function after delivery; dosage adjustments may be needed.
Hyperthyroidism: Watch for postpartum thyroiditis, which can occur in women with a history of Graves' disease.
Breastfeeding: Both levothyroxine and antithyroid medications are generally safe, but close monitoring of the infant’s thyroid function is advisable.
Thyroid problems during pregnancy require careful management to minimize risks to both the mother and the fetus. Regular monitoring, appropriate medication adjustments, and a multidisciplinary approach are key strategies to ensure a healthy pregnancy and optimal outcomes for both mother and baby.